Neonatal sepsis is a serious medical condition that occurs in newborns when there is an infection present in their bloodstream. It is a leading cause of morbidity and mortality in neonates, particularly in premature infants or those with low birth weight. Understanding the pathophysiology of neonatal sepsis is crucial for early diagnosis and effective treatment.
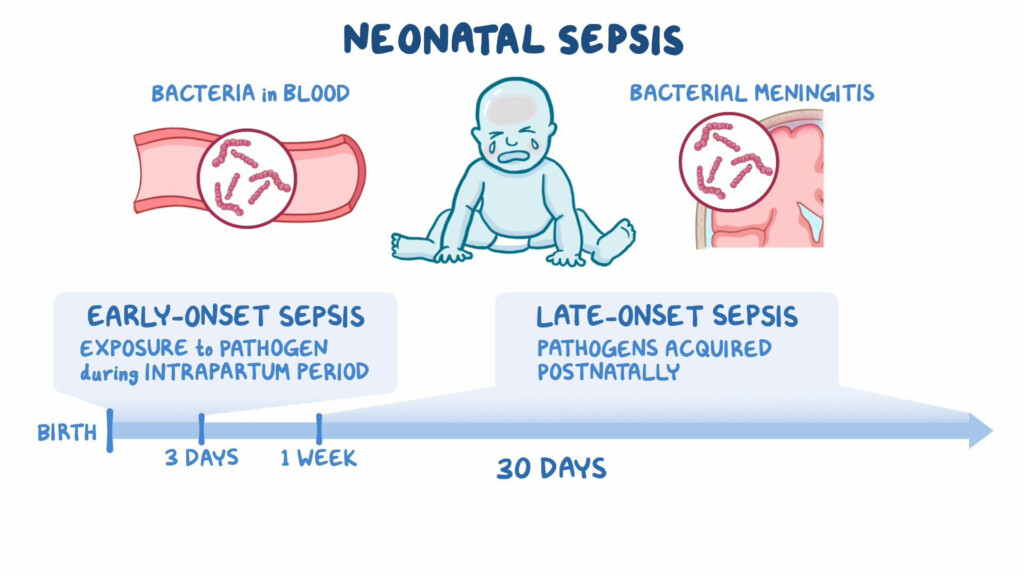
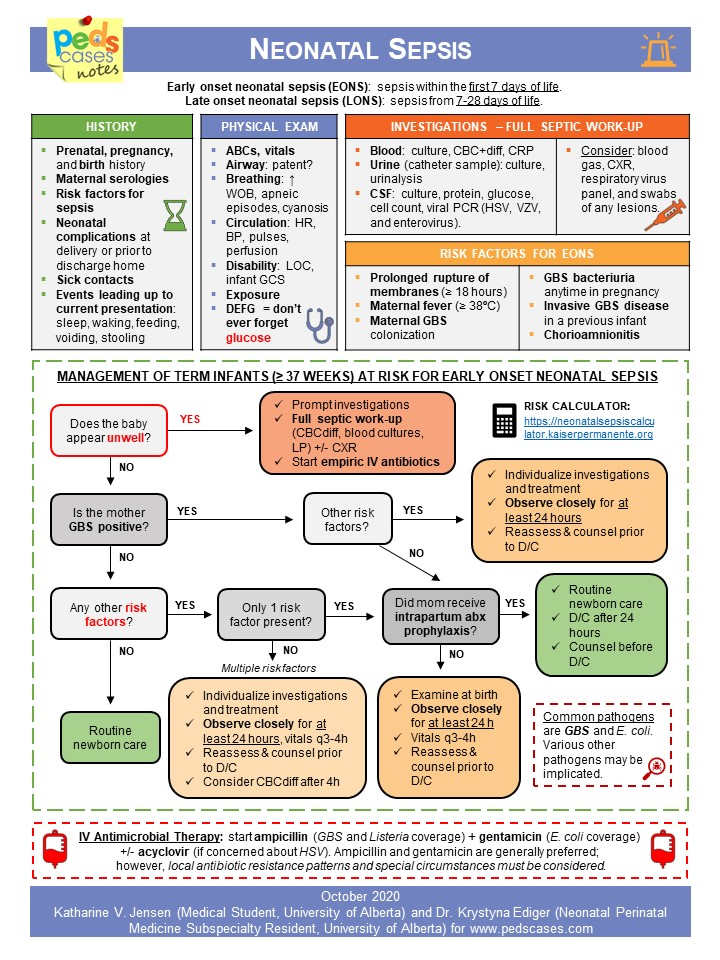
Neonatal sepsis can be classified into two main types: early-onset sepsis (EOS) and late-onset sepsis (LOS). EOS typically occurs within the first 72 hours of life, while LOS occurs after 72 hours up to 28 days of life. The pathophysiology of neonatal sepsis involves a complex interplay of host immune response, virulence factors of the pathogen, and various risk factors.
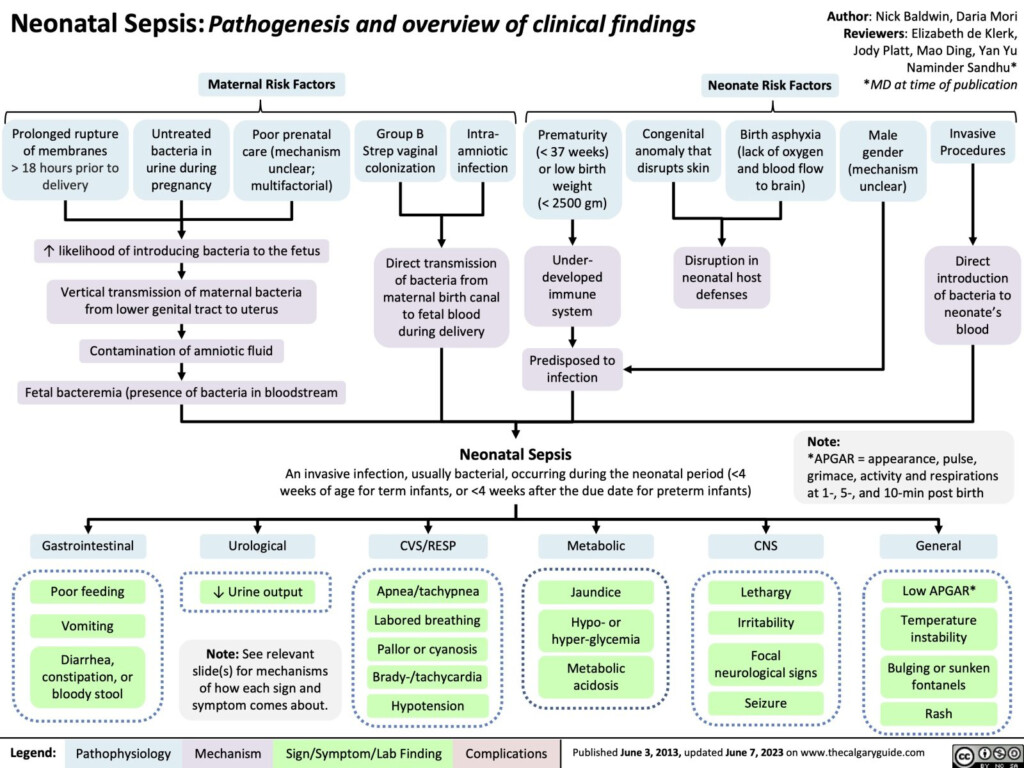
Flow Chart Pathophysiology Of Neonatal Sepsis
Pathophysiology of Neonatal Sepsis
The pathophysiology of neonatal sepsis begins with the entry of pathogens into the bloodstream, either through vertical transmission from the mother or nosocomial sources. The immune response of the neonate plays a crucial role in determining the severity of sepsis. In neonates, the immune system is immature, making them more susceptible to infections.
Once the pathogens enter the bloodstream, they trigger an inflammatory response, leading to the release of pro-inflammatory cytokines and activation of the coagulation cascade. This dysregulated immune response can result in systemic inflammatory response syndrome (SIRS) and progress to septic shock if not promptly treated. The presence of risk factors such as prematurity, low birth weight, invasive procedures, and prolonged hospitalization further increases the risk of neonatal sepsis.
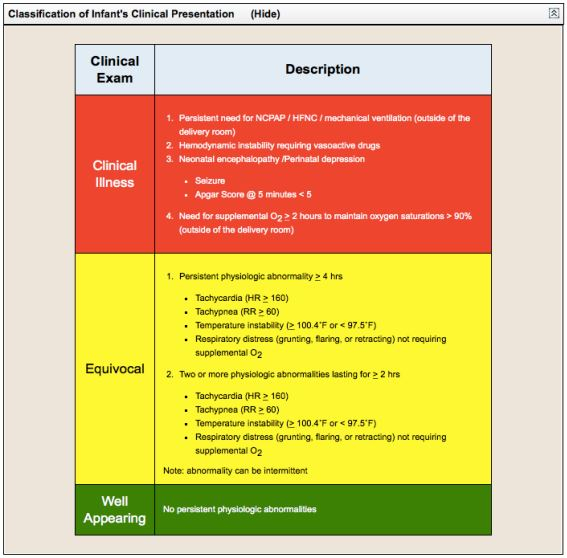
Clinical Presentation and Diagnosis
The clinical presentation of neonatal sepsis can vary depending on the age of onset and the causative pathogen. Common symptoms include fever, hypothermia, respiratory distress, poor feeding, lethargy, and jaundice. Diagnosing neonatal sepsis involves a combination of clinical evaluation, blood cultures, and laboratory tests. Early recognition and prompt treatment with antibiotics are essential to improve outcomes and reduce mortality rates.
In conclusion, understanding the flow chart pathophysiology of neonatal sepsis is crucial for healthcare providers involved in the care of newborns. By recognizing the early signs and risk factors, timely intervention can be initiated to prevent complications and improve outcomes for neonates at risk of sepsis.
Download Flow Chart Pathophysiology Of Neonatal Sepsis
Consensus Clinical Guidelines For Early Onset Sepsis EOS Screening
Neonatal Sepsis Calgary Guide
Neonatal Sepsis ForumIAS
Neonatal Sepsis PedsCases